Deep dives
Hospital at home
Hospitalization at home (HAD) is emerging as an innovative solution to the challenges of an aging population and the growing demand for personalized care. In 2025, this model is taking on a new dimension in Switzerland, driven by a desire for systemic transformation and the digitization of the healthcare system. It is also a concept that appeals to patients who have been able to test it.
This Deep Dive draws on the testimonies, feedback and analyses of Swiss and international experts gathered at the Digital Health Connect 2024 conference to provide an in-depth overview of the challenges, achievements and prospects of the home hospitalization model in Switzerland.
Home care in a context of demographic transition
Switzerland, like many countries, is experiencing a significant increase in its so-called “senior” population, with 19.4% of its population aged over 64 in 2024. This ageing is accompanied by an increase in degenerative and chronic diseases, putting hospital infrastructures under increasing pressure.
According to the CollHome study, the desire to grow old at home is widely shared by 90% of senior citizens. Between 2013 and 2022, the number of patients receiving home care has increased by 84%.
One of the solutions to this problem lies in conceptualizing the home as a care environment.
Chloé Schorderet, scientific assistant at the University of Applied Sciences and Arts Valais/Wallis
The “Hospital at Home” model: a paradigm shift
The concept of the hospital at home originated in the United States and is now well established in many countries.
Hospitalization at home involves hospital-level care and infrastructure, including specialized medical and nursing staff, digital solutions that facilitate the transmission of shared data and telemedicine, acute examinations and treatments, as well as high-quality standards.
Being at patients’ homes implies a change of approach.
The idea is to move hospital care to the home and provide acute care treatment there in a multidisciplinary manner, in partnership with external stakeholders.
Laura Treccani, member of the board of directors of the Swiss Hospital at Home Society
Laura Treccani is convinced of it: “Hospital-at-Home is not only a response to the Covid-19 pandemic, but also a real transformation of the care model.
Some caregivers have to take off their shoes before entering. The degree of ‘power’ is thus different.
Henrik Bjärtun, specialist in internal medicine and co-founder of the start-up Medoma
Feedback: three pilot projects in Switzerland
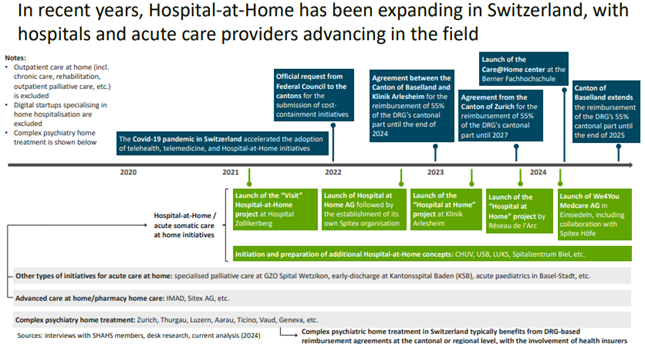
In Switzerland, several establishments have launched pilot home hospitalization projects, thus laying the foundation for a structural change in patient care, as shown in the infographic of the Swiss Hospital at Home Society below.
Three initiatives, led by committed actors, concretely illustrate the possibilities and challenges of the model:
Hospital-at-Home at the Arlesheim Clinic
- Basel-Landschaft
Since its launch, this project, which has become a fully-fledged service, has treated 290 patients in 18 months, with three daily visits, including one interprofessional visit, combined with remote monitoring.
It emphasizes the importance of allowing patients to choose between hospital and home, of adapting hospital protocols and of adapting to the specific needs of patients, which are key elements for the success of this transition.
It’s about finding people who like this new approach and who dare to think differently.
We4You in Einsiedeln
- Schwytz
The We4You network, based in Einsiedeln, is based on an integrated holistic approach and interdisciplinary collaboration.
Her ambition is to break down professional silos and build a common culture of care. She advocates for decompartmentalization of healthcare professions, a rethinking of traditional practices, and a refocusing on coordination around the patient. She emphasizes the need to train the new generation of caregivers to approach the care relationship differently.
Claudia Günzel, director of the Spitex Höfe care network in the Pfäffikon region, points out that the success of such projects depends on better communication between the various stakeholders and the importance of integrating home services such as Spitex.
The patient tells us what they need and we discuss what we should do.
Dr. Kerstin Schlimbach, doctor in charge of We4You
Patient@home at the Biel Hospital
- Bern
Through the Patient@home project, the Biel Hospital Center (CHB) aims to provide certain acute care services directly to patients’ homes. The system provides for 24/7 monitoring via a digital platform, provided by CHB doctors using telemedicine, while on-site care is provided by partners such as home care services (ASD).
It reiterates the importance of sharing knowledge and emphasizes the need to settle the issue of invoicing and pricing, with the collaboration of the health insurance funds.
Let’s not reinvent the wheel separately, but work together.
Gianni Imbriani, Head of the Project Management Office at the Centre Hospitalier de Bienne
The advantages of hospitalization at home
Home care encourages changes to infrastructure, while also making it possible to include new digital technologies. Primary care and doctors continue to play an essential role.
Improvement of the quality of life of patients
Hospital at Home allows patients to receive care in a familiar environment, contributing to their psychological well-being and faster recovery. Patients retain their autonomy and maintain their social ties, which are essential factors for their overall health.
A study from February 2025, conducted at the University Clinic for Child and Adolescent Psychiatry and Psychotherapy of the University Psychiatric Services Bern (UPD) and the University of Bern, emphasizes that therapy at home is more effective than a stay in a clinic. The young patients treated at home as part of the AT_HOME pilot project had significantly fewer psychiatric symptoms than those who received treatment in a hospital setting.
Patients feel better and safer at home.
Henrik Bjärtun, specialist in internal medicine and co-founder of the company Medoma
According to him, thanks to home hospitalization, patients are also more involved in their care and have a better understanding of their condition, while sleeping and eating better.
Reduction of healthcare costs
Hospital at home has economic advantages in that it reduces the length of hospital stays and the number of readmissions, thus contributing to better management of hospital resources.
A study published in Nature Medicine in 2022 showed that up to 40% savings are possible thanks to lower infrastructure costs and shorter treatment times.
Case Study: Saving thousands of days of hospitalization
During the 12th edition of the Digital Health Connect conference. Prof. Daniel Lasserson, Consultant Physician in the Department of Geriatric Medicine at the John Radcliffe Hospital at Oxford University Hospitals, explains that for the 3,000 patients treated by his team in the United Kingdom, 14,000 days of hospitalization have been saved, representing approximately 800,000 pounds sterling for a single hospital in one year. The death rate during home treatment is also very low, and the home hospital also makes it possible to provide care during the last year of life, when 80% of medical expenses are incurred.
Prevention of nosocomial infections
In Switzerland, 6% of patients contract an infection in hospital. By avoiding prolonged hospital stays, HAH reduces the risk of nosocomial infections, a major public health issue as highlighted by this research from the University Hospital of Madrid.
The challenges of home hospitalization
Several challenges arise when home hospitalization is considered. The major obstacles are: change management and reimbursement.
Interprofessional collaboration
Interprofessional collaboration remains a major challenge in the context of home care.
Providing home hospitalization care relies on close collaboration between doctors, nurses, occupational therapists, pharmacists and other stakeholders.
But in French-speaking Switzerland, the CollHome study, led by the HES-SO Valais-Wallis, reveals that exchanges are too often limited to the transmission of information, without any real systematic coordination. Among the obstacles identified are working outside the institution, lack of time, lack of recognition for collaborative activities and the persistence of rigid professional hierarchies.
There is an evolution in the caregiving function: doctors and caregivers are joining forces in an integrated collaboration and seeing a transformation of their role, with less medical hierarchy.
Laura Treccani, member of the board of directors of the Swiss Hospital at Home Society
We have put forward several hypotheses. Among them, the fact of working outside an institutional structure seems particularly decisive.
Chloé Schorderet, HES-SO Santé Valais/Wallis
The results do indeed show that professionals who are part of the same organisation collaborate more. This observation is confirmed by scientific literature.
In addition, other factors can influence the quality of interactions: the availability and accessibility of colleagues, but also the very perception of what constitutes “good collaboration”, which can differ between professions. Another review revealed that doctors and nurses do not always share the same criteria for evaluating the quality of their cooperation.
Reimbursement for home hospitalization: a barrier to overcome
Despite the demonstrated clinical and economic benefits, the biggest obstacle is certainly related to the fact that, in Swiss health insurance law, reimbursement for such care is not provided for. To date, no standardized national tariff covers this type of care. This considerably hinders the development of the model, forcing each pilot project to find solutions on a case-by-case basis, often through individual negotiations with insurance companies, cantons and certain support funds.
The objective would be to create new DRG (Diagnosis Related Group) packages adapted to such acute home care, which requires a political mandate, supported by evidence of the medical and economic effectiveness of the model. This data exists, but now it needs to be integrated into the decision-making process.
Within the Swiss Hospital at Home company, a working group is discussing this pricing issue. In particular, we are trying to get closer to other players, to develop models that we can present to the political world.
Laura Treccani, committee member of the Swiss Hospital at Home company, created in 2023 to promote this concept
Innovations and futurs prospects
Technological innovations play a crucial role in home care. They not only guarantee the safety and quality of care, but also standardize practices, streamline coordination between stakeholders and facilitate patient empowerment.
For HAH to be a credible alternative to traditional hospitalization, examinations must be able to be carried out at home. The emergence of portable technologies for radiology, ultrasound or biological analyses now makes it possible to bring immediate and mobile diagnostic capacity to patients’ homes.
In a well-organized HAD service, an ultrasound, ECG or PCR test can be performed at home in less than an hour.
Prof. Daniel Lasserson, Oxford University Hospitals

Remote monitoring: remote surveillance and medical IoT
Advances in the medical Internet of Things (IoT) enable continuous monitoring of patients at home. Intelligent sensors can now monitor vital signs and remotely alert healthcare professionals in case of abnormalities.
In a well-organized HAD service, an ultrasound, ECG or PCR test can be performed at home in less than an hour.
Prof. Daniel Lasserson, Oxford University Hospitals
Several Swiss start-ups are at the forefront of these technologies:

Artificial intelligence for monitoring
A pilot project, led by the Réseau de l’Arc jurassien as part of the Swiss Center for Care@home, in partnership with the University of Bern and the Danish company WARD Project, is exploring whether home care for patients suffering from heart failure is feasible. Remote monitoring would be carried out using devices equipped with artificial intelligence that could predict a possible deterioration in the state of health, triggering rapid intervention by the care team and an adaptation of the treatment and care plan.
Palliative emergency home or virtual units
Patrizia D’Amelio, head of the Geriatrics and Geriatric Rehabilitation Department at the CHUV in Lausanne, estimates that 30 to 40% of geriatric inpatients could be cared for at home. (source:)
In Fribourg, the canton has put out for consultation a long-term care planning report for the period 2026-2030.
The Geneva University Hospitals (HUG) launched a palliative home emergency service in 2025. This service aims to offer urgent palliative care 24/7 to end-of-life patients, directly in their homes.
International inspiration: virtual wards
In Germany, the Asklepios hospital group is setting up virtual wards in nursing homes, inspired by the “Hospital@Home” models of the British and US National Health Services, where “Virtual Wards” became established during the Covid-19 pandemic.
These units provide continuous monitoring, video consultations and digital coordination of teams.
Conclusion
Hospitalization at home represents a major development in the provision of healthcare in Switzerland. This model offers a promising solution to meet the challenges of an ageing population and the growing demand for personalized care.
In hospital, the patient’s autonomy is taken away, with a gown and appointments. Patients spend a lot of time waiting.
Dr. Henrik Bjärtun, Medoma
In Switzerland too, we have to get away from the idea that the hospital solves all problems. It solves some, but sometimes it creates others. This does not mean that everyone should be hospitalized at home, but that this solution should be offered to those for whom it would be of interest.
Patrizia D’Amelio, Head of the Geriatrics and Geriatric Rehabilitation Department at the CHUV
Home hospital care offers personalized care that is often well received by patients and their families, while also having obvious medical benefits.
However, its success depends on the ability to overcome the challenges of interprofessional collaboration, skills adaptation and the integration of digital technologies.
The future of HAH in Switzerland relies on a holistic approach, combining medical expertise, technological advances and enhanced collaboration between all actors in the healthcare system. By adapting care models, the benefits of offering high-quality, patient-centered care are gained, while optimizing the use of healthcare resources.
The future of healthcare will involve a more decentralized, digital and human organization, with the hospital at home as the essential model.